VAGINAL CANCER
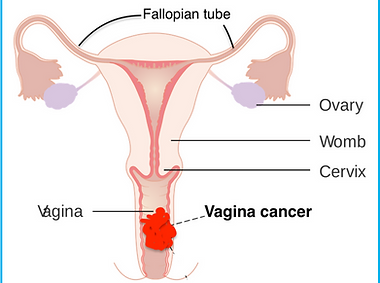
Vaginal cancer is a rare type of cancer that forms in the tissues of the vagina, the muscular tube connecting the uterus to the outside of the body. It most commonly affects the cells lining the surface of the vagina, called the vaginal epithelium. Like other cancers, it occurs when abnormal cells grow uncontrollably, forming tumors that can potentially spread to other parts of the body.
Types of Vaginal Cancer
The most common types of vaginal cancer include:
- Squamous Cell Carcinoma: This is the most common form, accounting for about 85% of vaginal cancer cases. It develops in the thin, flat cells lining the vagina and usually grows slowly.
- Adenocarcinoma: This type starts in the glandular cells of the vaginal lining. It is less common than squamous cell carcinoma but is more likely to spread to distant parts of the body.
- Melanoma: Melanoma, more commonly known as a skin cancer, can develop in the pigmented cells of the vagina. Vaginal melanomas are very rare.
- Sarcoma: Sarcomas develop in the deeper tissues of the vaginal wall, such as muscle or connective tissue. These cancers are also quite rare.
What are the causes of Vaginal Cancer?
The exact cause of vaginal cancer is not known, but several risk factors can increase a woman’s chances of developing the disease:
- Human Papillomavirus (HPV) Infection: HPV, a sexually transmitted virus, is a major risk factor for vaginal cancer, particularly squamous cell carcinoma. Persistent infection with high-risk HPV strains (like HPV 16 and 18) can lead to abnormal cell changes in the vagina, which may develop into cancer over time.
- Age: Vaginal cancer is more common in older women, particularly those over the age of 60.
- History of Cervical Cancer or Precancerous Changes: Women who have had cervical cancer or precancerous changes in the cervix are at a higher risk of developing vaginal cancer.
- Diethylstilbestrol (DES) Exposure: Women whose mothers took DES (a synthetic form of estrogen) during pregnancy to prevent miscarriage are at increased risk of developing a rare form of vaginal cancer called clear cell adenocarcinoma.
- Smoking: Smoking increases the risk of vaginal cancer, particularly when combined with an HPV infection.
- Weakened Immune System: Women with weakened immune systems, such as those with HIV/AIDS or those taking immunosuppressive drugs, have a higher risk of vaginal cancer.
Symptoms of Vaginal Cancer?
In its early stages, vaginal cancer may not cause noticeable symptoms, which can make early detection difficult. However, as the cancer progresses, symptoms may include:
- Unusual vaginal bleeding (especially after intercourse, between periods, or after menopause)
- Watery vaginal discharge
- Pelvic pain or pain during intercourse
- A lump or mass in the vagina
- Painful urination or frequent need to urinate
- Constipation or difficulty with bowel movements
What tests will be required for diagnosis?
Diagnosis of vaginal cancer often involves:
- Pelvic Examination: A manual and visual exam to check for abnormalities in the vagina.
- Pap Test: While primarily used for cervical cancer, it can sometimes detect vaginal cancer cells.
- Biopsy: A sample of tissue from the suspected area is taken to confirm the presence of cancer cells.
- Imaging Tests: Tests such as MRI, CT scan, or PET scan may be used to determine if the cancer has spread.
Vaginal Cancer Treatment
Treatment for vaginal cancer depends on the stage and type of cancer and may include:
- Surgery: Surgery is often used to remove localized tumors. In some cases, part of the vagina may need to be removed (partial vaginectomy) or, in more advanced cases, a total removal (radical vaginectomy) may be necessary.
- Radiation Therapy: Radiation therapy is often used either alone or after surgery to kill remaining cancer cells. It can also be the primary treatment for advanced or inoperable cancers.
- Chemotherapy: Chemotherapy may be used in combination with radiation therapy or when cancer has spread to other parts of the body.
- Targeted Therapy and Immunotherapy: These treatments, which target specific cancer cell mechanisms or boost the body’s immune system to fight cancer, are being studied and used in some cases, depending on the cancer’s characteristics.