UTERINE CANCER
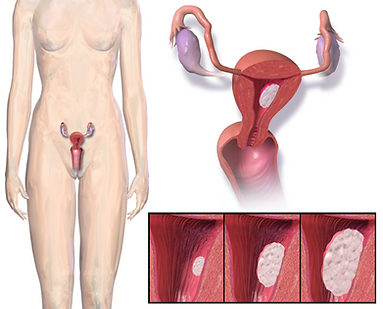
Uterine cancer, also known as endometrial cancer, is a type of cancer that begins in the uterus, specifically in the lining of the uterus called the endometrium. The uterus is a hollow, muscular organ where a fetus develops during pregnancy. Uterine cancer is the most common cancer of the female reproductive system and usually occurs in postmenopausal women.
Types of Uterine Cancer
The two main types of uterine cancer are:
- Endometrial Carcinoma: This is the most common type, accounting for about 90% of uterine cancer cases. It arises from the cells of the endometrium. Endometrial carcinoma is further classified into several subtypes based on histological characteristics, with endometrioid carcinoma being the most prevalent.
- Uterine Sarcoma: This is a rarer form of uterine cancer that arises from the muscle and connective tissues of the uterus (the stroma). Uterine sarcomas are generally more aggressive and have a poorer prognosis compared to endometrial carcinomas.
What are the causes of Uterine Cancer?
While the exact cause of uterine cancer is not fully understood, several risk factors are associated with an increased likelihood of developing the disease:
- Hormonal Factors: Estrogen Exposure: Women who are exposed to high levels of estrogen, whether from hormone replacement therapy, obesity, or certain medical conditions, have an increased risk. Prolonged unopposed estrogen exposure (not balanced by progesterone) can lead to the thickening of the endometrium, raising the risk of cancer.
- Age: Uterine cancer is most commonly diagnosed in women over the age of 50, particularly during or after menopause.
- Obesity: Excess body weight is a significant risk factor, as fat tissue produces estrogen, leading to higher levels of the hormone in the body.
- Diabetes: Women with type 2 diabetes are at a higher risk of developing uterine cancer, possibly due to associated obesity and hormonal imbalances.
- Family History: A family history of uterine cancer or other cancers (such as breast or colorectal cancer) can increase risk. Genetic conditions like Lynch syndrome (hereditary non-polyposis colorectal cancer) are also associated with a higher risk of uterine cancer.
- Menstrual History: Irregular menstrual cycles, early onset of menstruation, or late menopause may increase the risk due to prolonged exposure to estrogen.
- Nulliparity: Women who have never been pregnant (nulliparous women) may have a higher risk of uterine cancer.
- Tamoxifen Use: Women who take tamoxifen for breast cancer treatment may have an increased risk of developing uterine cancer, as the drug can have estrogen-like effects on the endometrium.
- Uterine Cancer Treatment: Treatment for uterine cancer depends on the stage of the disease, the type of cancer, and the patient’s overall health. Common treatment options include:
- Surgery: The primary treatment for localized uterine cancer usually involves a hysterectomy, which is the surgical removal of the uterus. In some cases, the ovaries and fallopian tubes may also be removed (salpingo-oophorectomy).
- Radiation Therapy: Radiation therapy may be used after surgery to kill any remaining cancer cells or as a primary treatment for advanced stages. It can be delivered externally or internally (brachytherapy).
- Chemotherapy: Chemotherapy may be recommended for advanced or recurrent uterine cancer. It involves the use of drugs to kill cancer cells or stop their growth.
- Hormone Therapy: Hormonal treatments may be used for certain types of uterine cancer that are hormone-sensitive, particularly in women who cannot undergo surgery.
- Targeted Therapy: For specific subtypes of uterine cancer, targeted therapies that focus on specific genetic mutations or pathways may be considered.
What tests will be required for diagnosis?
Diagnosis of uterine cancer typically involves several steps, including:
- Pelvic Examination: A physical examination to check for abnormalities in the uterus and surrounding areas.
- Transvaginal Ultrasound: This imaging test uses sound waves to create images of the uterus and can help identify abnormalities.
- Endometrial Biopsy: A sample of tissue from the endometrium is taken and examined for cancerous cells. This is often the definitive test for diagnosis.
- Dilation and Curettage (D&C): In some cases, a D&C may be performed to obtain a larger tissue sample for testing.
- Imaging Tests: CT scans or MRI may be used to determine if cancer has spread beyond the uterus.
Uterine Cancer Symptoms
Symptoms of uterine cancer may be vague and similar to those of other conditions. Common symptoms include:
- Abnormal vaginal bleeding: This can include bleeding between periods, heavy menstrual bleeding, or bleeding after menopause.
- Unusual vaginal discharge: Any unexpected discharge, especially if it’s blood-tinged, should be evaluated.
- Pelvic pain: Pain or discomfort in the pelvic area that is new or worsening.
- Weight loss: Unexplained weight loss can occur as the disease progresses.
- Pain during intercourse: Discomfort or pain during sexual activity may also be a symptom