CERVICAL CANCER
Cervical cancer is the second-most common cancer in women worldwide, particularly affecting women between the ages of 30 and 45. It is primarily caused by the human papillomavirus (HPV), a common sexually transmitted infection. HPV can cause changes in the cells of the cervix, which can be detected through screening tests like the Pap smear. If these changes are not identified and treated, they may develop into cancer over time.
What makes cervical cancer unique is that it is one of the few cancers that can be prevented through vaccination (HPV vaccine) and regular screening tests. This dual prevention strategy helps catch abnormal cell changes early, reducing the chances of the disease progressing to cancer.
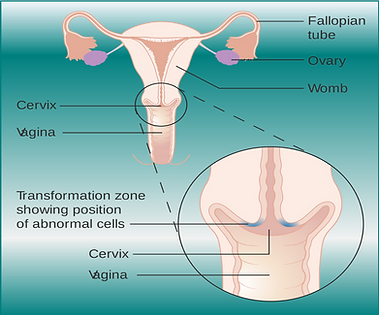
Where is cervix situated in the body?
The cervix is located in the lower part of the uterus, which is the organ where a baby grows during pregnancy. It acts as a narrow, cylindrical passage connecting the uterus to the vagina (birth canal). The cervix plays an important role in various functions, such as allowing menstrual blood to pass from the uterus into the vagina and opening during childbirth to allow the baby to pass through. It is also the area where cervical cancer can develop.
What are the causes?
The primary cause of cervical cancer is infection with certain strains of the human papillomavirus (HPV). However, there are other factors that may contribute to the development of cervical cancer in combination with HPV infection. Here’s a breakdown of the major causes and risk factors:
1. Human Papillomavirus (HPV) Infection
- HPV is the leading cause of cervical cancer. There are many types of HPV, but the most dangerous strains linked to cervical cancer are HPV 16 and HPV 18. HPV is a sexually transmitted virus, and most sexually active individuals are exposed to it at some point.
- While most HPV infections resolve on their own, some persistent infections with high-risk strains can lead to abnormal changes in cervical cells, potentially developing into cancer if untreated.
2. Weakened Immune System
- Women with weakened immune systems, such as those with HIV/AIDS or those taking immunosuppressive drugs (e.g., after organ transplants), are at a higher risk of HPV infections progressing to cervical cancer. Their bodies may struggle to fight off infections like HPV.
3. Smoking
- Smoking increases the risk of cervical cancer. Tobacco by-products have been found in the cervical mucus of women who smoke, which can damage the DNA of cervical cells, making them more vulnerable to HPV infection and cancerous changes.
4. Sexual Behavior
- Multiple sexual partners or having a partner with multiple sexual partners increases the risk of HPV infection, which can lead to cervical cancer.
- Early sexual activity (starting intercourse at a younger age) also increases the risk of HPV exposure.
5. Long-term Use of Oral Contraceptives
- Long-term use of birth control pills (more than five years) has been linked to an increased risk of cervical cancer. The reason for this is not fully understood, but the risk decreases once the pills are no longer used.
6. Having Many Pregnancies
- Women who have had three or more full-term pregnancies may have a higher risk of developing cervical cancer, though the reason behind this link is not fully understood. Some theories suggest that hormonal changes or a weakened immune system during pregnancy might contribute to the risk.
7. Infrequent or Lack of Screening
- Not getting regular Pap smears or HPV tests can lead to missed detection of abnormal cervical cell changes, which can progress to cancer if untreated.
8. Family History of Cervical Cancer
- Having a family history of cervical cancer may increase a woman’s risk, suggesting there may be some genetic susceptibility to the disease.
9. Exposure to Diethylstilbestrol (DES)
- Women whose mothers took the drug DES (a synthetic form of estrogen) during pregnancy to prevent miscarriage are at a higher risk of developing a rare type of cervical cancer.
What are the symptoms?
Cervical cancer often does not show symptoms in its early stages. As the disease progresses, symptoms may appear, including:
- Unusual vaginal bleeding (after intercourse, between periods, or after menopause)
- Pelvic pain
- Pain during intercourse
- Unusual vaginal discharge